The Most Important Things to Know About Diabetes


What is diabetes?
Diabetes is a chronic condition that, on the most basic level, develops when too much glucose (blood sugar) is circulating in your body. To illustrate how this happens, let’s start with a little physiology. We get glucose from two sources: the foods and drinks we consume and the body’s built-in supplier, the liver.
If your glucose level dips—say, between meals—then the liver converts glycogen (a form of sugar stored in the body) into glucose for an energy boost. In order for that glucose to get distributed to the body’s cells and get to work, though, we need a hormone called insulin (made by the pancreas)to help transport it.
When you have diabetes, however, your pancreas may not produce enough insulin. Or it does produce enough insulin, but your body just doesn’t respond to it. In fact, “most people who have type 2 diabetes actually have very elevated insulin levels,” says Dr. Shabina Ahmed, M.D., an endocrinologist and an assistant professor of medicine at Johns Hopkins University, in Baltimore.
As a result, you wind up with an excess of glucose in your bloodstream, which, if left unchecked, can lead to inflammation, triggering additional health issues.
What are the types of diabetes?
Type 1 diabetes
Type 1 diabetes (T1D) is an autoimmune condition with a strong genetic link. In people with type 1, an overactive immune system attacks the pancreas, damaging its insulin-producing cells (known as beta cells) until they no longer make enough insulin to manage blood sugar levels. Because of the genetic predisposition and the underlying autoimmune component, T1D is typically diagnosed in childhood (you may have even heard it referred to as juvenile diabetes), but an increasing number of people are getting diagnosed in adulthood. Recent epidemiological data have shown that more than half of new T1D cases occur in adults. (More on the rise of adult-onset T1D in a minute.)
Type 2 diabetes
With type 2 diabetes (T2D), your pancreas can produce enough insulin, but your body is insulin-resistant, meaning it can’t absorb and use glucose properly—the result of a perfect storm of genetic and lifestyle factors, such as carrying excess weight and living a sedentary lifestyle. The most common form of the disease, T2D affects up to 95% of all people with diabetes. It's often referred to as adult-onset diabetes, but just as the rate of T1D in adults is escalating, so, too, is the rate of T2D in children, rising 4.8% per year between 2002 and 2015, according to SEARCH for Diabetes in Youth, a national multicenter study.
Prediabetes
Often considered a precursor to T2D, prediabetes means your blood sugar is elevated, but not yet elevated enough to be considered diabetes. According to the Centers for Disease Control and Prevention (CDC), an astounding 96 million Americans have prediabetes—but one in three don't even know they have it.
“When you have prediabetes, your blood sugar levels are not necessarily going to be consistently high,” says Dr. Joshua Miller, M.D., the medical director of diabetes care at Stony Brook Medicine, in New York, and an associate professor of endocrinology and metabolism at Stony Brook University. “And so you may not be symptomatic.” Meaning the most likely way to get a diagnosis is through a regular checkup with your doctor, like an annual physical and corresponding blood tests. While prediabetes puts you at a higher risk of developing T2D, it isn't inevitable: Consider it a heads-up to prioritize healthy habits and get blood sugar levels back on track.
Gestational diabetes
As the name suggests, this type of diabetes occurs during pregnancy—which also means it’s temporary. When someone is pregnant, their placenta produces hormones that can cause higher levels of glucose in the blood. In roughly 10% of women, this leads to insulin resistance and excess blood sugar. Luckily, gestational diabetes typically goes away after delivery, but it can be a precursor to prediabetes and/or T2D.
The good news is that gestational diabetes should be routinely screened for during the second trimester, per guidelines by the American College of Obstetricians and Gynecologists. This is key, as untreated gestational diabetes can lead to premature birth and stillbirth.
What are the risk factors for diabetes?
Risk factors for type 1 diabetes
It’s not clear why the immune system overreacts in T1D, but researchers believe it’s due to a mix of genetic and environmental factors: “We know that something triggers the immune system to attack the pancreas,” says Miller. “I think it’s a combination of having a baseline risk and an environmental trigger.”
That trigger, notes Miller, can happen at any age, which could explain the rise in adult-onset cases. T1D may potentially be set off by viruses (including COVID-19) and stressors such as surgery, and it can also occur when the pancreas is damaged or removed due to another health condition, such as chronic pancreatitis. A family history of T1D and other autoimmune diseases can also up your risk; “you may have a family member with hypothyroidism or multiple sclerosis—autoimmune diseases tend to run in families, but they don’t always present in the same way,” says Ahmed.
Risk factors for type 2 diabetes
Like T1D, experts believe both genetics and environmental triggers play a large role in T2D. “If you talk to someone with T2D, they will probably tell you of at least one relative who also has the disease,” says Ahmed. But having a genetic predisposition doesn’t mean you’ll definitely develop the disease. Other factors raise your risk, including:
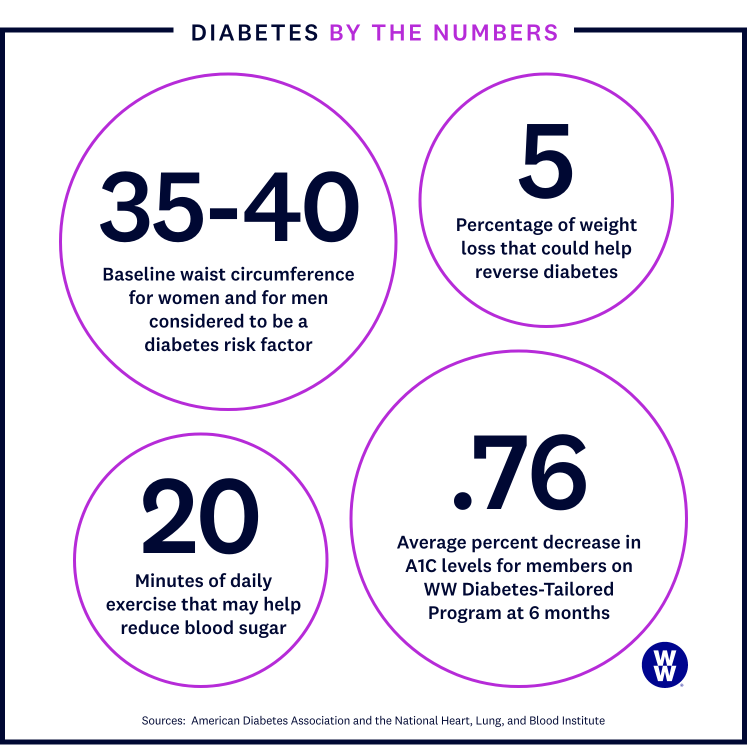
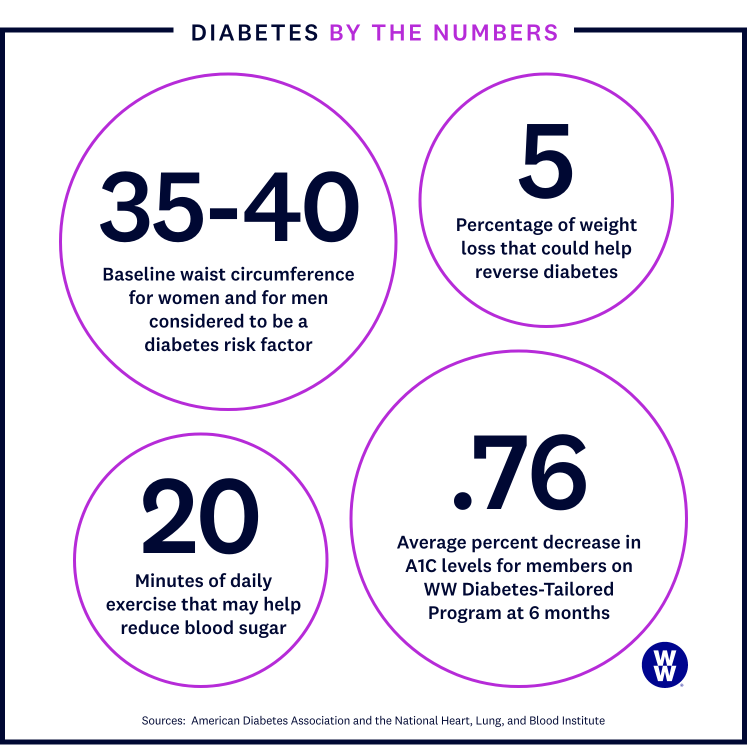
- Excess weight. Living with excess weight (a BMI, body mass index, between 25 and 29.9) or obesity (30 or greater) can lead to insulin resistance, particularly if that weight is concentrated around your midsection. According to the National Heart, Lung, and Blood Institute, a waist circumference greater than 35 inches in women and greater than 40 inches in men is considered a risk factor. That’s because belly fat can indicate visceral fat, the kind that wraps around your internal organs and causes inflammation. This could be one reason why T2D is more common in men than women, as men tend to have higher amounts of visceral fat.
- Lack of activity. Research has long established that a sedentary lifestyle increases your risk of developing T2D. For example, the more time men spent sitting, the more likely they are to develop T2D, one study in the International Journal of Behavioral Nutrition and Physical Activity found.
- Age. Diabetes is more likely diagnosed in those 45 and older (although, as mentioned, juvenile cases of T2D are on the rise).
- Related conditions. A personal or family history of prediabetes, gestational diabetes, cardiovascular disease, high blood pressure, and/or high cholesterol ups your risk of T2D.
- Race. Black Americans, Latin Americans, American Indians, and Alaska Natives are at a greater risk of developing T2D than other ethnic groups—partly due to genetic factors but also due to broad health inequities that are systemic and persistent. A review published in Diabetes Care showed that unsatisfactory access to both healthcare and healthy foods and a dearth of safe areas for physical activity play a role in why people of color, Indigenous people, and individuals with low income are at a higher risk of developing T2D.
- Tobacco use. Research shows that smoking may increase the risk of T2D, as it may increase insulin resistance.
Risk factors for prediabetes
Since prediabetes can act as a precursor to T2D, the risk factors are primarily the same, including family history, lack of physical activity, and excess weight.
Risk factors for gestational diabetes
If you previously had gestational diabetes, gave birth to a baby over nine pounds, or were overweight (a BMI higher than 25) before your current pregnancy, you’re more likely to develop gestational diabetes. Other risk factors include:
- Prediabetes
- A family history of diabetes
- Another condition that affects insulin, such as polycystic ovary syndrome (PCOS)
- One or more other health conditions, such as high blood pressure
Your blood sugar levels should return to normal after you give birth, but having gestational diabetes does put you at a higher risk of developing T2D; according to the CDC, 50% of women with gestational diabetes wind up with the condition later on.


What are the symptoms of diabetes?
While there are different types of diabetes, the signs and symptoms are the same, and that’s true for both men and women. If you're experiencing any of the below, it's time to check in with your doctor.
- You're peeing more than usual. When blood sugar levels are elevated, your kidneys notice and try to filter out the excess. They're working overtime, sending you to the bathroom a lot more than usual. How much more exactly? “We’ve had patients say they’re going hourly,” says Miller.
- You're (very) thirsty. Due to the increased urination, you may be dehydrated. And being dehydrated may make you thirsty. And being thirsty may make you drink more. And drinking more may make you urinate more. (And the cycle continues.)
- Increased hunger. You ate just 15 minutes ago, but you're already feeling starved. What gives? Your muscles and other tissues aren't getting their necessary dose of glucose, so they're telling your brain that they're hungry even if you’re freshly nourished.
- You're tired. Like fall-asleep-at-your-desk tired. Extreme fatigue is a classic sign of diabetes. Again, because all that glucose, a prime energy source, isn't getting where it needs to go. (Plus, the dehydration doesn’t exactly help you feel energized.)
- You're losing weight. When your body isn't getting enough glucose for fuel, it may break down fat and muscle in order to produce glucose. And that can cause a drop on the scale. This tends to happen more with T1D than T2D.
- You're seeing double. Blurry vision happens when the lenses of your eyes swell due to too much blood sugar.
- Minor cuts take forever to heal. Critical genes involved in tissue repair are suppressed in those with diabetes, according to a study in Nature Communications. This means even slight wounds can take a long time to recover and can be vulnerable to infection.
- You have tingles. High blood sugar can damage nerves, leading to tingling, pain, and numbness in the hands and feet. It's more common in those with T2D but can occur with T1D.
It's worth noting that for some people, the symptoms of T2D are so mild that many don't even know they have the disease; according to the CDC, an estimated one in five people with diabetes don’t know they have it. Likewise, prediabetes and gestational diabetes often occur without symptoms, so many people aren’t initially aware they have these conditions.
How can diabetes be prevented?
Researchers don’t know enough about T1D yet to advise on how to prevent it—or whether it’s even preventable. The story differs for prediabetes or T2D. Research shows that even losing just 5% to 7% of your body weight (that's 10 to 14 pounds for a 200-pound person) reduces your risk of developing T2D.
One way to do that is through a customised weight-loss programme. In a clinical trial in the American Journal of Public Health, the WW programme helped adults with prediabetes lose weight and significantly improve their blood sugar levels at six and 12 months, staving off T2D.
How is diabetes diagnosed?
Doctors rely on several blood tests for diabetes—the fasting blood sugar test being the most common of the bunch. This test measures the amount of glucose in your blood after an overnight fast (i.e., not eating). The scoring goes like this:
- A blood sugar level of 99 mg/dL (milligrams per deciliter) or less is considered normal.
- Between 100 and 125 mg/mL (milligrams per milliliter) is prediabetes.
- Anything over 125 mg/mL indicates diabetes.
Your physician will likely check your A1C levels too. Sugar binds to the hemoglobin in your blood, so if your blood sugar levels are elevated, your A1C levels will be too. The A1C test gives doctors an average of your blood sugar levels over three months.
- An A1C level under 5.7% is considered normal.
- Anything between 5.7% and 6.4% is prediabetes.
- A level of 6.5% and above means diabetes.
There's also an oral glucose tolerance test, often used to diagnose gestational diabetes. During this test, your blood sugar levels are measured in regular intervals over three hours after you drink a glucose drink.
- A blood sugar level of 140 mg/dL or lower is normal.
- From 140 to 199 mg/dL is gestational prediabetes.
- A level of 200 mg/dL and above is gestational diabetes.

Tell Me More About...Thirst
Q: You mentioned that thirst is a diabetes symptom, and I am in desperate need of some H₂O right now. Could it be diabetes?
A: If you’re feeling more parched than usual, you may worry you have diabetes, but don’t panic. The thirst associated with the disease, called polydipsia, is extreme. “It’s not a fleeting, ‘I have a dry mouth today’ or a ‘I’m a little bit thirsty’ thought—it’s constant thirst, all day long,” says Miller. And it comes with the urge to pee constantly, fruity breath, and fatigue from being so dehydrated.
Q: Right, but is there any way to quench it? How do you get un-thirsty?
A: Getting blood sugar under control is the obvious fix. “A big problem is that many people feel thirsty and so they drink Gatorade or soda, and those sugary drinks only worsen the situation by raising blood sugar levels through the roof,” says Miller. That leads to more urination, more dehydration–it’s a vicious cycle.
Q: This sounds like a pretty substantial symptom. Is it the most common?
A: “No, the most common symptom is no symptom,” says Ahmed. Some people experience thirst and frequent urination, while others are asymptomatic. “People will say they feel perfectly fine, and then they’re diagnosed on routine blood work,” Ahmed says. That’s why annual screenings are a must.
What are the complications of diabetes?
When blood sugar stays elevated for too long, it leads to inflammation that damages your organs. How long is too long? On average, about 10 years. Here’s what can happen over years and decades when glucose levels go untreated.
- Heart disease. Because of the damage to blood vessels, people with diabetes are at a higher risk of heart attack or stroke.
- Kidney disease. Diabetes is the leading cause of kidney disease. And severe disease can lead to dialysis. Your doctor will monitor a patient’s urine for protein to watch kidney function.
- Eye issues. People with diabetes are also referred to an ophthalmologist at the time of diagnosis and continue to go biannually or annually.
- Diabetic ketoacidosis (DKA). This severe complication is more common in those with T1D. Cells starved for glucose (because there isn't enough insulin to get glucose to the cells) turn to fat for energy. This process creates a chemical by-product called ketones. When ketones build up in the blood, it becomes acidic. In severe cases, this can lead to diabetic coma (losing consciousness for long periods) and even death.
- Hand and foot problems. Nerve damage, known as diabetic neuropathy, occurs in about a third of diabetes patients. It can lead to pain, numbness, and tingling in the hands and feet. Also, stagnant blood flow means minor cuts (often in the feet) can heal poorly and may cause a severe infection that, in some cases, can lead to amputation. High blood sugar levels can also invite fungal infections—vaginal yeast and fungal nail infections are common in people with diabetes.
- Skin issues. Often a symptom of elevated blood sugar levels, skin conditions can manifest in a variety of ways, including necrobiosis lipoidica (pimple-like bumps that progress into swollen, hardened patches), skin tags (hanging skin growths), and diabetic dermopathy (dark spots or lines that create an impression in the skin, typically on the shins), as well as blisters, dry patches, and open wounds that result from poor circulation.
- Gum issues. Periodontitis, an infection of the gums and bone that hold teeth in place, occurs more frequently in people living with diabetes, as does dry mouth and thrush (a fungal infection).
What is the best diabetes treatment?
Your treatment will depend on your type of diabetes and its severity. Are you destined to be on meds? Not necessarily. Your physician will push lifestyle changes, which may help stave off meds. “If a patient’s blood sugar levels aren’t too high when newly diagnosed, I’ll give them three months to turn things around through diet and exercise,” says Ahmed. “If they have moderate to high hyperglycemia [high blood sugar], then we'll do lifestyle changes plus medication right away,” she adds. Here are the treatment options.
Lifestyle changes. Diet and exercise alone can't reverse T1D, but healthy eating, exercise, and prioritizing sleep can help you better manage the disease and its symptoms. For patients with T2D, eating well, exercising, and losing weight may help you avoid medications, including insulin.
For people with T2D who are overweight or have obesity, the recommendation from the American Diabetes Association and the International Diabetes Federation is to lose at least 5% of your weight and keep it off. "Weight loss is very unlikely to happen with exercise alone," says Ahmed. Exercise has been shown to reduce insulin resistance, but you'll need to make dietary changes if your goal is to lose weight.
Insulin. With T1D, your pancreas doesn't produce enough insulin, so supplementing with insulin is a must. However, insulin is less common in treating T2D. Insulin can be taken in a few different ways:
- A self-administered injection via a syringe or a pen
- An insulin pump, which delivers the insulin required throughout the day via a catheter
- An inhaler containing a powdered form of insulin
Oral medications. Several oral drugs can help lower blood sugar and A1C levels, including:
- Metformin (a.k.a. Glucophage, Glumetza, Fortamet, or Riomet): This is often the first line of defense for diabetes. It slows the breakdown of glucose from foods and reduces how much glucose your liver produces.
- SGLT2 inhibitors (Farxiga, Invokana, Jardiance): These help the kidneys remove sugar from your blood. Bonus: They've been shown to help lower blood pressure.
- DPP-4 inhibitors (Januvia, Onglyza, Tradjenta): This med class stimulates the pancreas to produce more insulin.
- GLP-1 receptor agonists (Victoza, Ozempic, Trulicity): These newer drugs lower blood sugar, reduce the risk of cardiovascular disease, and help patients lose weight.
Is there one diet that’s best for people with diabetes?
Experts say no. You don't have to go no- or low-carb to manage your diabetes (phew!). Still, reducing your intake of carbohydrates—particularly processed, sugary foods—while boosting your fiber intake (which includes beans, peas, and lentils) is helpful. High-fiber foods break down more slowly, so your system doesn't get the flood of glucose that comes from sugar-laden foods.
If you need help prioritizing quality, whole foods, WW’s PersonalPoints™ Programme is a customised science-based plan to help you lose weight while still eating the foods you love.
What about exercise?
Exercise can also help reduce blood sugar and A1C levels. Those with T2D who work out regularly tend to have better blood sugar control than those who don’t, a 2020 study in Medicine & Science in Sports & Exercise showed. Here’s what you want to do.
- Move more, plain and simple. We already mentioned that being sedentary is linked to a higher risk of T2D. Even just moving your body in everyday activities—taking the stairs instead of the elevator, folding laundry, taking a work call while standing instead of sitting—can help.
- Aim for 150 minutes of exercise a week. When broken up over seven days, that's just a little over 20 minutes of movement a day. The general recommendation is moderate to vigorous activity (walking, biking, swimming…cleaning the bathroom—it all counts).
- Add resistance training. Research shows that working with weights, resistance bands, or even your body weight for 20 minutes two to three times a week can help you respond better to insulin and can aid in weight loss.
While diabetes is undoubtedly complex, getting it under control doesn’t have to be. By leveling up your diet, squeezing in more movement, and working in partnership with your doctor, you can help minimize the complications of diabetes, so you can feel your best—and live your best life possible.
Disclaimer
The WW programme and guidance are not intended as a substitute for medical diagnosis, treatment, or advice. You should always consult your healthcare provider about any healthcare issues.